Acute myeloid leukemia (AML) poses significant challenges in terms of prognosis and treatment options. Leukemic stem cells (LSCs) contribute to therapy resistance, relapse and adverse outcomes. This study aimed to explore one of the major features of LSCs (e.g. quiescence) and its underlying molecular mechanisms, as well as identify potential targets for therapeutic intervention.
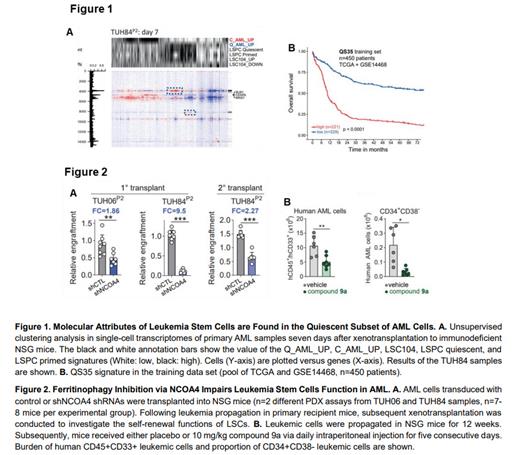
Using in vivo cell labeling in patient-derived xenograft (PDX) assays, we identified a quiescent cell subpopulation with high LSC potential. Transcriptomics experiments conducted separately on quiescent and cycling cell subsets revealed gene signatures characteristic of quiescent (Q_AML_UP) and cycling cells (C_AML_UP). Using single-cell RNA sequencing, we identified clusters of quiescent leukemic cell that were highly enriched in gene signatures related to LSCs (Figure 1A). Through a machine learning approach, we identified a gene set highly specific of quiescent cells (named the QS35 gene signature) that emerged as a significant prognostic factor for poor outcomes in independent cohorts of AML patients (Figure 1B).
Next, we aimed to identify new vulnerabilities of LSCs by investigating the quiescent subset of leukemic cells. Transcriptomics and proteomics approaches on quiescent vs cycling cells revealed enhanced autophagy within the quiescent subset. Additionally, the transferrin receptor TFRC and ferritin, two key regulators of iron metabolism, exhibited lower expression in the quiescent subpopulations. As intracellular iron availability is tightly regulated by ferritinophagy, a specific form of autophagy leading to the degradation of ferritin, we investigated the coordinated regulation of autophagy and iron metabolism in the quiescent LSC subset. Intriguingly, the intracellular iron pool was lower in quiescent LSCs, particularly in the CD34+CD38- compartment compared to more mature leukemic cells. Moreover, autophagy inhibition selectively induced cytotoxicity in the CD34+CD38- compartment and reduced the frequency of long-term culture-initiating cells (LTC-IC), and these effects were rescued by exogenous iron supply, underscoring the critical role of autophagy in iron bioavailability within the quiescent LSC subpopulation.
To target ferritinophagy in this compartment, we depleted NCOA4, the main carrier in ferritinophagy responsible for delivering ferritin-bound iron to the autophagosome, using shRNAs in primary AML samples. Interestingly, NCOA4 was found more expressed in quiescent compared to cycling AML cells. In ex vivo assays, NCOA4 downregulation significantly reduced the frequency of LTC-IC and inhibited the clonogenic capacities of leukemic cells. Furthermore, NCOA4 invalidation abrogated leukemia initiation and self-renewal in serial transplantation experiments in vivo, particularly within the quiescent LSC population (Figure 2A). Additionally, treatment with a novel small molecule inhibitor named compound 9a that disrupts the NCOA4-ferritin interaction, depleted intracellular iron in primary AML cells, reduced their clonogenic potential and LTC-IC frequency ex vivo, and induced cell death specifically within the quiescent CD34+CD38- subset. Importantly, the viability of LSCs treated with compound 9a was rescued by the addition of iron, demonstrating that the cytotoxic effects of this compound were dependent on iron depletion. Notably, compound 9a exhibited minimal toxicity to normal hematopoietic cells ex vivo. In PDX models, in vivo short-term treatment with compound 9a decreased tumor burden and induced cell death within the CD34+CD38- LSC population (Figure 2B).
Mechanistically, genetic of chemical inhibition of NCOA4 led to the accumulation of dysfunctional mitochondria, and to the generation of reactive oxygen species especially within the LSCs population. Furthermore, inhibition of NCOA4 by compound 9a decreased mitophagy, strongly suggesting that NCOA4 coordinates ferritinophagy and mitophagy pathways to increase intracellular iron, thereby specifically promoting the survival of LSCs.
These findings highlight the critical vulnerability of quiescent LSCs to ferritinophagy. Thus, NCOA4 inhibition represents an innovative therapeutic approach for AML patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal